Diane Russell’s hair began falling out the day before her second treatment. It was just 25 days after she learned she had breast cancer, and she was still grappling with the diagnosis.
She had noticed swelling, then lesions on her breast and thought she was suffering from an infection such as MRSA. As a medical professional at Roper Berkeley, she helped cancer patients. She never expected she would be one. “I didn’t think it was cancer,” Russell said, her eyes brimming with tears. “I never knew I’d be on the other side.”

Unlike many diseases, breast cancer can vary greatly in women. There are non-invasive cancers – those that do not need aggressive treatment – and invasive forms. According to Dr. Lynn Crymes of Lowcountry OB/GYN, “infiltrating ductal carcinoma is most common,” accounting for 70 percent to 80 percent of all invasive cancers.
Once a diagnosis is made – taking into account the type and grade of cancer cells as well as the presence of hormone and protein receptors – a team of doctors, including a radiologist plus medical and surgical oncologists, will determine a course of treatment.
Some women don’t want to wait until a tumor appears and are opting for pre-emptive treatment. Dr. Crymes said there has been lots of press about Angelina Jolie, who carries the BRCA gene mutation and opted for a double mastectomy. The BRCA mutation has been shown to “significantly increase” the risks of both breast and ovarian cancer. Women with a family history should have a candid conversation with their doctor about genetic testing.
“I have seen quite a few women who have lost mothers, sisters, aunts and grandmothers to early breast cancer,” Dr. Crymes said, adding that by determining the presence of the BRCA mutation “we are able to prevent these cancers and give women normal life expectancies.”
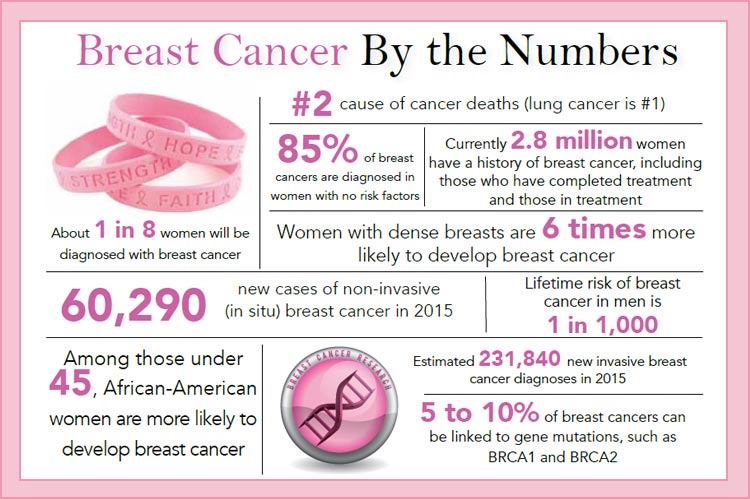
Mammograms are advised for women over 50, although many doctors feel strongly that 40 would be a better starting point. Mammograms can detect many tumors, but, because they are two-dimensional images, they may miss them in very dense breasts or appear to indicate a tumor where none exists, resulting in additional testing.

Fortunately, there’s a new game in town, and it will change the way breast cancer is diagnosed. Dr. Amy Bethea, a radiologist with Roper St. Francis, is excited about tomosynthesis.
“It will be in each of our of breast centers in September,” Dr. Bethea said. “Instead of the two-dimensional mammogram images, we’ll have three-dimensional “sweeps” of each breast.”
She added that not all patients will be candidates at first – until tomosynthesis becomes the standard – but she predicted that it will decrease the call-back rate and increase the early diagnosis rate.
Sitting in a recliner receiving infusion therapy at the Roper Cancer Center, Diane Russell spoke candidly about her feelings, how different it is to suddenly be the recipient of care instead of being the caregiver and the emotional moment when she realized she was beginning to lose her hair. It used to be long, but she had it cut so the loss wouldn’t feel quite so traumatic.

Russell realizes she is in good hands at the Roper Cancer Center. She has an excellent oncologist that she likes, and the staff is dedicated to meeting her needs and making sure she is comfortable. With the opening of the Donna Fielding Cancer Wellness Institute at Roper, patients can receive help that goes far beyond surgery, radiation and infusion therapy.
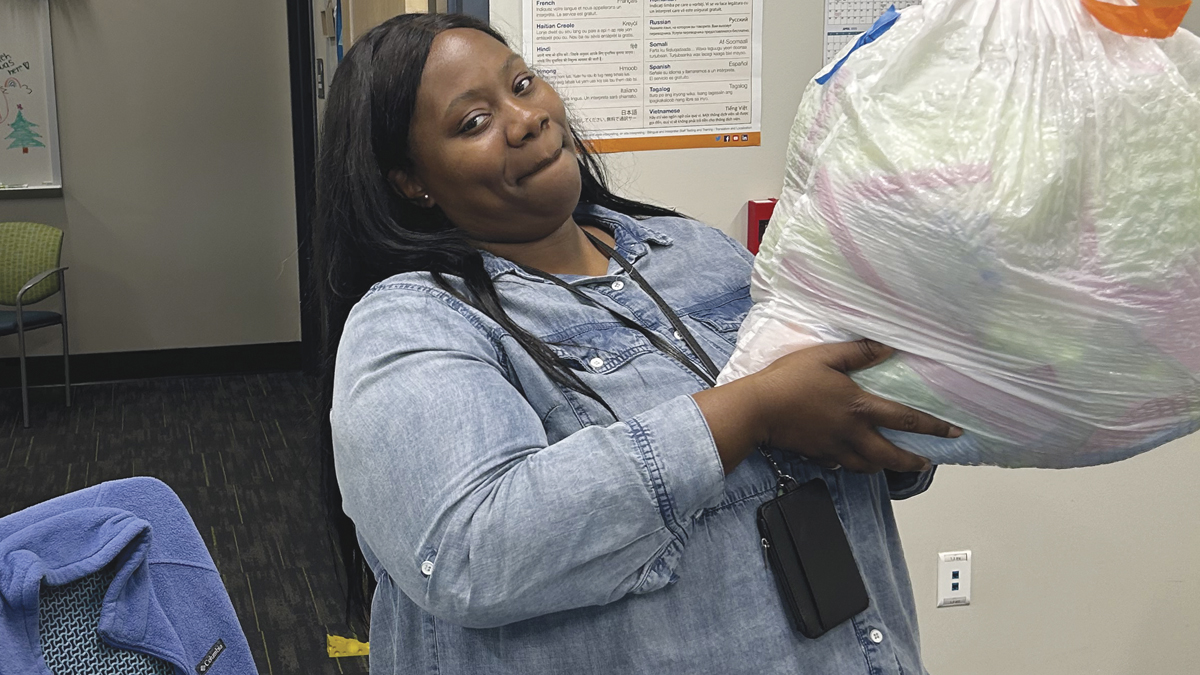
Jody McCrain is a wellness navigator – one of several – who provides information and resources as well as a comfortable environment for patients and their families. Wellness navigators, some of them breast cancer survivors themselves, know the ropes and can offer guidance as well a hug or a few minutes to vent.
The Cancer Center also features a small café, as well as The Healing Boutique, which features beautiful adornments (hello retail therapy!). The boutique also offers specialty items and fittings for mastectomy patients and private consultations for wigs. In addition to support groups, massage therapy by licensed practitioners and nutrition classes are among the services available to patients and even employees – because wellness and prevention go hand-in-hand.
“Breast cancer is the second most common diagnosis in women,” according to Dr. Crymes, adding that the death rate from breast cancer has declined by about 20 percent over the last 10 years, the result of improvements in therapy and earlier detection through increased screening.
A breast cancer diagnosis is a journey into the unknown. But thanks to advancements in detection and treatment, more women are not only surviving but thriving. Just as important, there are wonderful people helping women every step of the way to a cure.
A breast cancer diagnosis is a journey into the unknown. But thanks to advancements in detection and treatment, more women are not only surviving but thriving. Just as important, there are wonderful people helping women every step of the way to a cure.
By Barbara Millen Patrick