When Raquel first began intensive cancer treatment, she wanted to focus all her energy on her treatment, but she quickly found herself facing a side effect she didn’t expect.
“My anxiety was as real and tangible as nausea and tiredness. Focusing on my breath slowed my fearful thoughts and distracted me from physical pain often. It also helped to slow down racing thoughts, relaxing me mentally and physically, as a quiet mind helps relieve tension in the body,” said Raquel, a Charleston resident who requested that her last name not be used. “I clung to ‘In through the nose, out through the mouth,’ as my chest would rise and fall and, eventually, I would drift into a quiet place. No stress. Just breathe.”
Raquel is one of about 30% of adults using health care approaches that are not typically part of conventional medical care as they explore ways to ease their pain and stress while navigating cancer.
Patients may find comfort in complementary treatments such as meditation, yoga, guided imagery, reflexology, massage and guided mindfulness. These practices sometimes help to manage symptoms and side effects of treatment and are meant to be used with and support other treatment.
According to the American Cancer Society, some people may find they can take a lower dose of pain medicine when they also use nonmedical treatments, but it’s important for patients to talk with their doctor and cancer care team to know if these may be good options for them.
Kallison Graham MSW, a social worker with Bon Secours St. Francis Cancer Care, works with patients who are at many different points in their cancer journeys.
“We find that mindfulness exercises help to create a calm mind, reduce stress and help patients focus on their treatment goals,” said Graham. “I have a personal belief that an anxious mind cannot exist in a relaxed body. When I see patients focusing on their breathing, I know that they are not going to focus on anything else during those moments.”
Mindfulness practice is considered a mind-body approach to care, like meditation, relaxation, deep breathing and yoga. Other approaches include body-based practices: massage; energy force therapies such as tai chi and reiki, and expressive therapies such as journaling and art therapy.
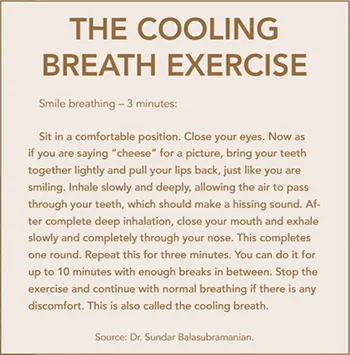
Dr. Sundar Balasubramanian provides inspiration and instruction surrounding breathing practices. He is an associate professor at the Medical University of South Carolina, a cell biology researcher and a certified yoga therapist, working with patients and faculty at the Hollings Cancer Center and the MUSC Health & Wellness Institute.
In his research, Dr. Balasubramanian explores the effects of yoga breath work and is studying its role in improved health benefits and treatment outcomes. He grew up in India and was familiar with yoga practices there, and he enjoys sharing his expertise.
“These practices are not focused in one religion or belief system. They can benefit individuals from many backgrounds and cultures,” he said.
At the Hollings Cancer Center, his focus is on yogic breathing for cancer patients. He is involved with MUSC’s Survivors’ Fit Club, a 10-week exercise, nutrition and behavior change program for breast cancer survivors. He teaches breathing exercises that can not only improve how patients feel emotionally but can also encourage physical improvements in health.
“Breathe a bit better!” is the title of Dr. Balasubramanian’s upcoming book, and that brief phrase encapsulates his belief that the lessons he teaches are not complicated and that anyone can learn how to practice the breathing exercises.
“People take breathing for granted, but, as people become more aware of their breathing, they can benefit from these practices in many ways,” he pointed out.
Another technique Graham uses is thought journaling. She asks patients to jot down times when they are having negative thoughts, and, when they bring these notes back to her, they work together to learn what triggers these thoughts and how they can change some of these thought patterns.
Wendy Edgin, a massage therapist at Olive Massage in Mount Pleasant, has extensive experience working with cancer patients.
“People come to me from many backgrounds – some who are taking a traditional approach to their cancer treatment and some who are going more holistic,” she said. “I listen to their medical history in detail. I respect where that person is in their treatment plan, and I focus on being helpful in their journey, where they are and where they want to be.”
 Depending on a person’s pain level on a certain day, a therapist may offer massage or simply “hold space” for them, which means being fully present. Some clients see Edgin on a regular basis, and some come only once or twice.
Depending on a person’s pain level on a certain day, a therapist may offer massage or simply “hold space” for them, which means being fully present. Some clients see Edgin on a regular basis, and some come only once or twice.
“My approach is to be here when you need me,” she said.
A seasoned oncology massage therapist, Lucy Allen is the founder of Oncology Massage of the Carolinas. She emphasized that getting to know her clients before they begin therapy is key to working with any client.
“Recognizing a patient’s background is especially important when people are dealing with cancer treatment due to any medications and side effects, organ dysfunction, bone fragility and other complications,” Allen explained. “After I take in all of their information, I set up a specific treatment plan for that person, understanding their risk factors and other considerations like their energy level.”
Since stress and anxiety can strike at any time, family members and caregivers may find benefit in participating with the patient in these methods. Dr. Balasubramanian teaches classes in breathing at the Hope Lodge in Charleston, a free home-away-from-home for cancer patients and their caregivers. When he teaches classes there, he finds that family members can learn along with their loved ones. Not only are they able to help the patient use the breathing practices when they get home, but they often find benefit for themselves as well.
At Oncology Massage of the Carolinas, Allen agrees that there is often a benefit to including caregivers: “When possible, I encourage family members to watch and follow along when I work with a patient so when I’m not with them, there are some massage techniques they may be able to do on their own.”
While the journey is different for each person, Edgin finds great satisfaction in being able to “give a healing touch, taking away some of the pain that medications can’t or don’t touch.”
By Lisa Wack