“It’s in your genes” is a common expression often used to describe a person who shares a personality trait or profession in common with a parent. These are typically innocuous familial connections that may help explain the origin of an individual’s passion or talent in a particular pursuit, but we can also inherit harmful genes that increase our risk of developing diseases such as cancer.
“Cancer is a genetic disease,” explained Kevin Hughes, MD, FACS, director of cancer genetics at the Medical University of South Carolina and director of the MUSC Hollings Cancer Center Hereditary Cancer Clinic, which offers patients with hereditary cancer syndrome a centralized location to get counseling, testing, screening, diagnosis and treatment. “So all cancer occurs when the genetics of that particular cell stop working properly, and the cells multiply uncontrolled and they go out to places they don’t belong. Those are called somatic mutations, the mutations that occur in the genes after you’re born and through your lifetime. Your germ line genes are the ones that you inherit from your parents, and some of those genes help protect us from cancer because they help prevent our DNA from going bad –from having a problem or mutation. These germ line genes can sometimes have a mutation that stops them from protecting the DNA.”
We have two sets of genes, one from our mother and one from our father, so half of each set of genes comes from each of our biological parents. Hereditary cancer, which is passed down through a family through inherited genetic mutations from a parent, accounts for 10% of all cancers.
Dr. Hughes used the analogy of brakes on a car. “You usually have two sets of these genes, and each one is like a cellular brake preventing cancer. You have to lose both copies for that cell to go on and develop a cancer, but, if a person is born with only one good copy and one bad copy (genetic mutation), that one good copy is the only thing protecting them. It’s like driving around with only one set of brakes. So that person or that cell can go on to develop cancer much more frequently than they would normally.”
Assessing Hereditary Cancer Risk
Mikayla Jennings, MS, a cancer genetic counselor with Greenwood Genetic Center in Greenwood, South Carolina, said there are specific factors to evaluate in determining a person’s hereditary cancer risk, based on either a personal diagnosis of cancer or family history.
“Often what we are thinking of for hereditary cancer are cancers diagnosed at a young age – typically for things like breast or colon cancer under the age of 50. Other things would be specific factors of the cancer they were diagnosed with. For example: breast cancer. We’re looking at was it triple negative, and then for prostate cancer we’re looking at was it metastatic or high grade or very high grade. And those are some clues that maybe there is something hereditary in the family.”
She continued: “And for the family, we’re looking at how many individuals in the family have been diagnosed with cancer; how many have been diagnosed with the same type or similar types of cancers.”
Jennings said the overarching goal of cancer genetic counseling is to help people “make an informed decision on whether they would like to proceed with genetic testing, as well as to provide them with a risk assessment. Just based on their personal and family history, what is the likelihood of there being something hereditary versus it not being hereditary.”
If genetic testing revealed an inherited gene mutation, that person would not necessarily develop cancer but would have a higher-than-average risk of having to deal with the disease. About 60% to 80% of people with the BRCA1 gene mutation, which leads to breast and ovarian cancer, contract breast cancer, while the rest don’t.
With other cancers – lung cancer, for example – we know that smoking compounds that risk. “So there are some factors like that that can exacerbate the gene, such as a gene that increases the risk of melanoma,” said Dr. Hughes. “When the patient goes out and gets a lot of sunburns, they’re more likely to get a melanoma than someone else with the same gene who doesn’t do that. But, in general, we don’t really know what it is that triggers the cancer in these patients that have mutations.”
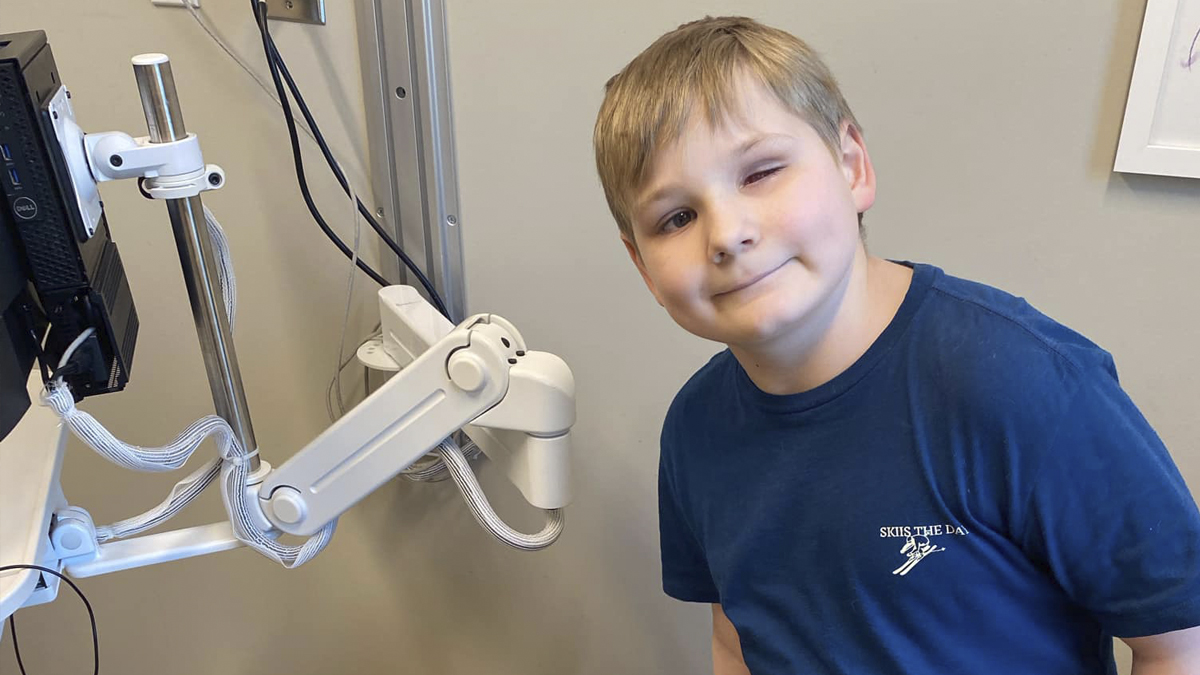
The recommended age for genetic testing depends on the gene and the age of onset, added Dr. Hughes. Although rare, some genes, such as the APC gene, cause cancer in children. With that gene, testing begins between the ages of 10 and 12. “We kind of pick the testing based on when the patient’s going to benefit from that testing. A good rule of thumb is 25. Because that’s when things really start changing in terms of risk. But it varies with the gene,” he said.
Ideally, testing should begin sooner rather than later so cancer can be discovered early or even prevented. “So for some cancers, like cancer of the breast, we have great screening for that,” asserted Dr. Hughes. “We have MRI, mammography – the two of those we find most cancers early and when they’re curable.”
Techniques to Test for Hereditary Cancer
One novel opportunity being offered through MUSC is its In Our DNA SC program, in which anyone older than 18 can get free genetic testing done as part of an 11-gene panel test that screens for hereditary breast and colon cancer risk and familial hypercholesterolemia. Dr. Hughes recommended that even those without a family history of cancer participate in the initiative.
“For those with a strong family history of cancer in the family – young age at diagnosis, many cancers in the family – those patients need full genetic testing, the full panels, but the In Our DNA covers a lot of other patients as well,” emphasized Dr. Hughes. Interested individuals can register at web.musc.edu/inourdnasc.
Another unique approach the Hollings Cancer Center uses is that once genetic testing reveals a gene mutation, the clinic follows up long-term with that individual. “By doing that, we’re increasing the compliance with the NCCN (National Comprehensive Cancer Network) guidelines, and then we expect we’ll decrease the morbidity and mortality of cancer for those patients,” stated Dr. Hughes. A few other clinics around the country use this approach, and Dr. Hughes believes it eventually will become the norm.
Though genetic testing is important for identifying a higher likelihood of hereditary cancer, most cancers are sporadic, which means we don’t have a good explanation as to why they occur. However, as Dr. Hughes related, “For that small number, that 10% who are hereditary, we can say ‘you have this certain gene that increases your risk; that’s probably why you have the cancer.’ Once identified, they and their family can decrease their risk by following the guidelines.”
By Colin McCandless