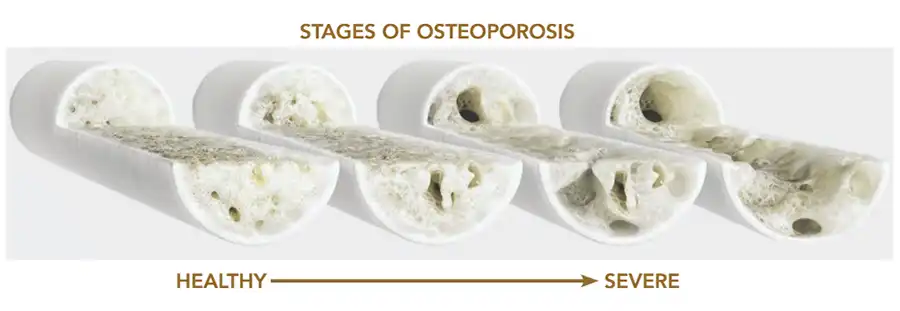
It’s so easy to forget that our bones are comprised of living tissue forever in a state of change as we age. The simple act of growing another day older can decrease our bone mass, making us more prone to fractures and osteoporosis.
Generally, people are prescribed a variety of ways to slow down this seemingly inevitable hurdle toward fragility: walk, run, lift weights, eat those leafy greens and other nutrient-dense foods to get our dose of Vitamin D.
The Case of Ms. Bruce: When Necessary Medication Comes with Risks
As women inch closer to menopause, they’re often advised to utilize the protective effect that hormone-balancing medications provide. They can do all these things to keep their skeletal foundations healthy and strong, but what happens when what makes women well adds to the burden of protecting those bones?
Despite doing everything they can to stay healthy, sometimes it’s just not enough and medical intervention is needed.
“I started taking levothyroxine some years back,” said Suzanne Bruce of West Ashley. “It was necessary when, after a long while of feeling fatigued and having other symptoms, I was diagnosed with hypothyroidism.”
That intervention certainly improved Bruce’s quality of life, but there are possible side effects of this necessary medication, one of which is osteoporosis.
Ignoring the Warning Signs: The Importance of Early Detection
Though Bruce’s medical provider had, over the years, gently nudged her toward a DEXA scan to measure her bone mineral density, she resisted. She wasn’t aware that both her condition of hyperthyroidism as well as levothyroxine can contribute to a loss of bone mineral density.
“I mean, I knew that I’d already had osteopenia, but I knew what my doctor would say after the scan: do weight-bearing exercises, eat your leafy greens, blah, blah, blah” Bruce groaned.
“I knew I just wasn’t going to do any of that,” she said, laughing, although she swore that she does, in fact, eat her vegetables.
Last year, however, Bruce went to her physician complaining of the sudden onset of off and on, inexplicable pain. She’d had no falls, bumps or spills, but much to her surprise, X-rays revealed compression fractures of her lumbar spine; the long-resisted DEXA scan became necessary. Bruce’s T-score, the measurement reflecting your bone mineral density compared with the average bone mineral density of a healthy adult of the same age was low, and Bruce was prescribed an injectable drug called Prolia.
“I don’t blame my osteoporosis on the levothyroxine,” Bruce said, “But I probably should’ve had that DEXA scan earlier. I might have avoided these fractures.”
“There were other factors at play, like my age, and I’m not sure it would’ve helped had I been aware that there was a risk of loss of bone mineral density, because, again, I didn’t want to hear about weight-bearing exercises and all that,” Bruce joked. “I do wish I’d been more vigilant.”
Long-term use of the following medications that may contribute to osteoporosis. If you’re on any of these, make time to talk to your doctor about measures you can take to stay ahead of loss of bone mineral density.
Medications and Bone Loss: Understanding the Link
Steroids
Because corticosteroids, such as prednisone and cortisone, interfere with the bone-rebuilding process, long-term utilization of them can lead to decreased bone density and increased risk of fracture.
Though steroids are most often used for a short duration, some patients, such as those suffering from Chron’s disease, asthma, psoriasis, or lupus, require longer treatment plans.
If you’re starting the journey of oral steroid use that will last three months or beyond, ask your physician for a bone mineral density test to gather a baseline and request a series of subsequent tests to keep an eye out for any change in density.
Proton Pump Inhibitors
Symptoms of heartburn can range from mild discomfort to a pain so severe you rush to the hospital, insistent that you’re mid-heart attack. For those of us who’d rather suffer this embarrassment than avoid our Nonna’s red sauce, PPIs have been heaven-sent.
Protecting us from acid reflux and soothing the guts of those with ulcers, PPIs are commonly found in medicine cabinets (and glove compartments and pocketbooks. . .) everywhere. However, those pesky studies keep ruining our lives by illustrating that long-term use of PPIs is — wait for it — associated with our body’s ability to absorb calcium, thereby increasing our risk of osteoporosis.
Antidepressants
Though antidepressant medications can greatly improve our quality of life, some types — particularly selective serotonin reuptake inhibitors (SSRIs) — have been linked to an increased risk of bone loss and fracture.
Adding to the risk of fracture for these patients is the nature of depression itself. Factors such as increased inflammation, behaviors such as the use of alcohol and tobacco, and a more sedentary lifestyle only seem to contribute to the environment perfect for snapping a bone or two.
Because the mechanisms of what causes SSRIs to contribute to bone loss and fracture are not fully understood, there seem to be no SSRI-specific ways to combat bone loss other than the general measures mentioned below.
Aromatase Inhibitors
Breast cancer, the second-leading cause of cancer-associated deaths in women, often includes years-long utilization of aromatase inhibitors. This category of drug including anastrozole, letrozole and exemestane adds years of disease-free living to survivor’s lives. Once again, this assistance comes at a cost.
Because this is a widely known issue, it’s doubtful that patients taking these medications are unaware of the risk. On the odd chance that your oncologist hasn’t discussed this specific risk with you, ask them about the widely established guidelines on monitoring, preventing and treating loss of bone density for those being treated with an aromatase inhibitor.
Universal Guidelines For Bone Protection
- Limit alcohol to no more than two drinks per day.
- Quit smoking.
- Do weight-bearing exercise.
- Take Calcium (1,200 to 1,500 mg/day)
- Take Vitamin D
Help to Heal
For some of us, long-term use of these drugs is unavoidable and in order to live a longer, healthier life, so is making that extra effort to preserve our bones. If you’re aware that a possible side effect of any long-term drug you’re taking is osteoporosis, vigilance is key. Requesting a DEXA scan, if it has not already been suggested, will at least give you a base line for comparison down the road.
If you don’t think you’re ready for a scan, ask your doctor about including the following markers in your next blood test:
- Vitamin D levels — Because adequate vitamin D levels are critical to good bone health, lower levels can indicate the status of your bone health.
- Bone-specific alkaline phosphatase — An estimate of the rate of bone formation over your entire skeletal system. Patients with osteoporosis generally have BALP levels that are up to three times normal.
- Urinary N-telopeptide of type I collagen, or uNTX — This can indicate bone resorption, or loss of bone.
By Amy Gesell