When thousands of South Carolinians are testing positive for COVID-19 every day and there are concerns that more contagious variants will speed up the spread of the coronavirus, a new treatment is offering hope to patients and hospitals alike.
Monoclonal antibody infusion therapy is an experimental treatment for COVID-19 patients at high risk of developing severe complications. In November 2020, the Food and Drug Administration issued an emergency use authorization for three monoclonal antibodies – bamlanivimab, casirivimab and imdevimab – to treat confirmed COVID-19 in high-risk patients with mild-to-moderate symptoms.
Trident Medical Center has been administering monoclonal antibody infusions since Nov. 30, and, according to Chief Medical Officer Dr. Lee Biggs, by the end of January, the hospital had treated more than 400 patients, with fewer than 2% of them requiring hospitalization, he said.
“The primary goal of the medication is to prevent hospitalizations by treating the most at-risk COVID-positive patients,” Dr. Biggs said. “It has provided a nice treatment option for those folks we know are at risk for requiring hospitalization. Over 98% of those we’ve treated were able to stay out of the hospital, so we like the benefit it delivers.”
Former President Donald Trump received Regeneron’s monoclonal antibody cocktail – which contains a combination of casirivimab and imdevimab – when he was treated for COVID-19 in October.
The website of the South Carolina Department of Health and Environmental Control lists Trident Medical Center as one of more than two dozen monoclonal antibody treatment locations in the Palmetto State.
A body that is invaded by a virus produces antibodies to fight it off. However, because the novel coronavirus that causes COVID-19 is new, it takes a while to produce enough antibodies to stop it from spreading. Monoclonal antibodies, which are grown in a laboratory, mimic the body’s natural antibodies.
Victims of the virus must receive treatment during the first 10 days of symptoms. On average, patients at Trident Medical Center have received monoclonal antibody infusions on their sixth symptomatic day. Dr. Biggs said most of those who eventually required hospitalization were closer to the 10-day limit.
“Time really is of the essence,” he said. “If anyone has viral-type symptoms, they should assume that it’s probably COVID and not a common cold or the seasonal flu. The sooner they get tested, the sooner we can treat them if they qualify.”
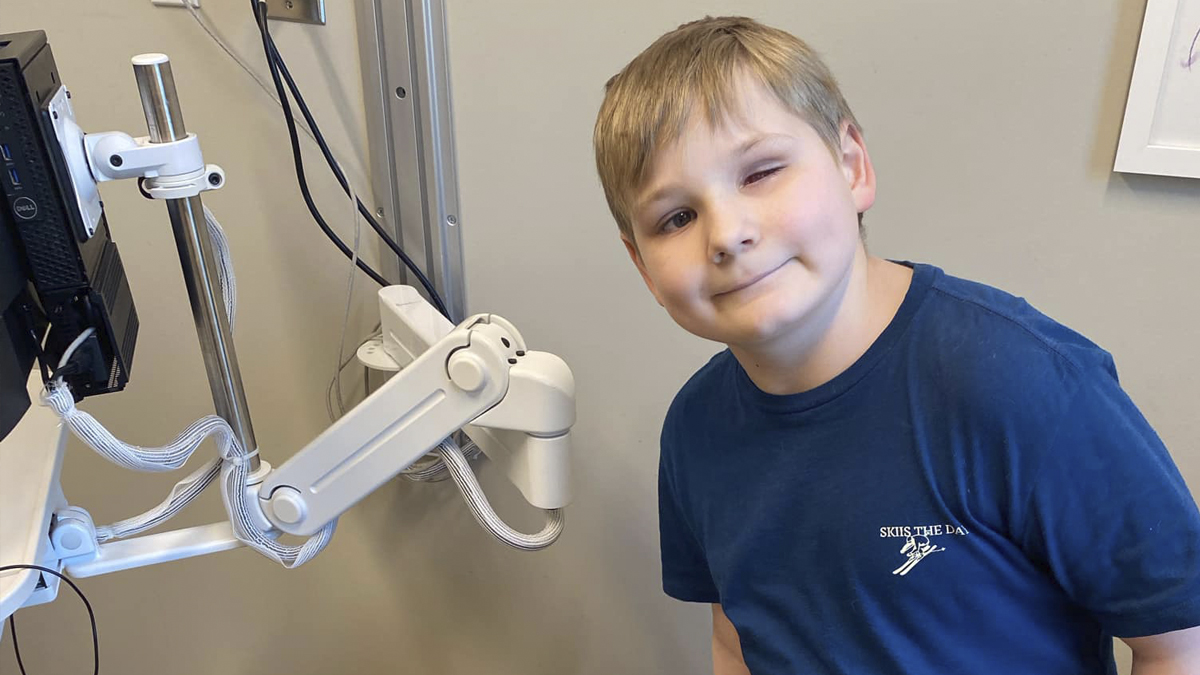
To qualify for monoclonal antibody treatment, patients must have tested positive for COVID-19 within the previous 10 days and not require oxygen. They must be at least 12 years old and weigh a minimum of 88 pounds.
Patients also must be at high risk for progressing-to-severe case of COVID-19. High-risk criteria include:
- A body mass index of at least 35;
- Chronic kidney disease;
- Diabetes;
- An immunosuppressive disorder;
- Currently receiving immunosuppressive treatment;
- Being 65 years or older;
- Being 55 years or older with cardiovascular disease, hypertension, chronic obstructive pulmonary disease or other respiratory diseases;
- Being 12 to 17 years old and having a BMI in the 85th percentile or greater for age and gender based on Centers for Disease Control growth charts; sickle cell disease; a congenital or acquired heart disease; neurodevelopmental disorders such as cerebral palsy; a medically-related technological dependence such as tracheostomy, gastrostomy or positive pressure ventilation not related to COVID-19; or asthma, reactive airway or other chronic respiratory disease that requires daily medication for control.
Trident Health identifies prospective monoclonal antibody patients through primary care providers and its five emergency rooms at Trident Medical Center, Summerville Medical Center, Brighton Park Emergency, Centre Point Emergency and Moncks Corner Medical Center. The three-hour treatment is administered at Trident Medical Center in space formerly used as a maternity wing.
Dr. Biggs said monoclonal antibody infusion therapy provides hospitals a treatment strategy it didn’t have last summer when cases surged.
“We were canceling elective surgical procedures because we needed that inpatient bed for a COVID patient. Maybe it was a person who just had their knee or hip replaced,” he said. “This treatment (monoclonal antibody infusion) has allowed us to continue to meet the health care needs of the community, be it procedurally or surgically, while managing this increased COVID demand.”
Dr. Biggs said one hospital stay is avoided for every 10 individuals receiving infusion therapy. He pointed out that at Trident Health, about 60% of COVID patients admitted to the hospital are Caucasian, while another 35% are Black or Hispanic.
When Trident first started offering monoclonal antibody therapy, about 90% of the patients were white. Trident has since seen a dramatic increase in minorities receiving the treatment, so much so that the number is closer to mirroring overall hospital admission percentages. Initially, Trident Health had difficulty getting the word out to minority populations, but word-of-mouth has helped spread the message, Dr. Biggs said.
“It’s not uncommon that we treat entire families,” he added.
Dr. Biggs said monoclonal antibody infusion therapy needs to be part of the overall strategy to fight COVID-19, along with vaccinations, masking, social distancing and hand-washing.
“COVID will continue to impact everybody’s life and health care well into 2021,” he said. “We need to continue to leverage all those strategies, and I think the antibody therapy is one that hasn’t been leveraged heavily enough.”