“So what are you going to do when you don’t like running anymore or your body gives out?” a family member asked me, only wishing, I was certain, to antagonize me.
“That can never happen,” I thought to myself – and I reassured that pesky relative that I was a capable, strong, determined, collegiate cross-country runner with miles to go.
Plot twist: Boy, was I wrong.
Late in my junior year of college, I grew more tired than I ever thought possible – sleeping 12-plus hours a night and crawling into bed as soon as I could after classes. My body ached – even carrying books across campus exhausted me. And, you guessed it, I no longer wanted to run. My body said no.
I’m not blaming my illness for my failure in a sport, but I am here to identify a chronic illness that has pushed my body to its limits and certainly has made me reprioritize and reset my health, wellness and fitness goals over the last six years.
What is this illness? An autoimmune disease – fibromyalgia. This is no regular disease: There is not finite test, and a person can appear completely fine one day or month while struggling to move or stay awake the next – hence earning the name, the “invisible disease.” It does not present the same face or identifying factors for any one person, so it’s increasingly hard to generalize the symptoms of fibromyalgia to the public.
While I know about my symptoms as a sufferer of fibromyalgia, I was able to speak with Dr. Antonio M. Hernandez, who is with Liberty Doctors, about how he is able to best help his patients. As an internist, he evaluates the patient entirely, looking for rheumatologic, neurologic and psychiatric history before making any decisions.
“Fibromyalgia could have overlapping psychiatric or neurologic presentations,” Dr. Hernandez explained. “A rheumatologist or a psychiatrist might see a patient with fibromyalgia differently.”
Once Dr. Hernandez is able to put the pieces of the patient’s puzzle together – these “pieces” often include blood testing, evaluating family history and a patient’s past medical history – he is able to make recommendations. Sometimes, that includes seeing a specialist.
“If a fibromyalgia patient presents with multiple joint pains, I’ll recommend to see a rheumatologist and rule out underlying autoimmune disorders like rheumatoid arthritis,” said Dr. Hernandez, providing an example.
Autoimmune disorders could present abnormal blood tests. Dr. Hernandez advises his patients with this disorder to check back in every four months for blood testing.
“If you have an underlying autoimmune disorder, make sure blood tests are routinely checked, especially the kidneys, because it is one of the most commonly affected organs,” he emphasized.
Another major item Dr. Hernandez checks off the list is vitamin levels. Vitamins D and B12 are important for bone, muscle and nerve health. Muscle aches, fatigue and bone pains can be symptoms of vitamin deficiencies. He also recommends taking fish oil supplements, stating, “It helps lubricate soft tissues of the joints and helps muscle and joint flexibility.”
Finding the right balance of supplements is important for just about anyone these days, but, for a patient with autoimmune disease, it is even more critical.
Concerning exercise and diet, Dr. Hernandez expressed his reasonable advice: “I don’t have a specific diet recommendation for patients with fibromyalgia. I just remind them to eat healthy, exercise regularly, eat a substantial amount of fiber daily, drink a good amount of water, and limit alcohol intake because it could cause muscle and joint pain due to inflammation. I also remind them to reduce activities that cause pain.”
One diet change that has proven successful for me, which Dr. Hernandez agrees with, is eliminating gluten. I’ve done this for the last three years, and it certainly helps keep inflammation and joint pain at bay.
Daily moderate exercise, with a focus on stretching, was his advice for getting the heart rate up – yoga being a great option.
Dr. Hernandez explained, “Stretching and yoga help blood flow better in the muscles and tendons, making them more flexible. The key to that is doing it daily and not overdoing it.”
My advice through all of this, bolstered by my conversation with Dr. Hernandez, is to find the right primary care doctor, particularly one specializing in internal medicine, to be your “home base.” This provider will probably know more about your body than you or Google knows. And that means you’re in good hands. Your most important job is to keep your health care provider informed about things such as skin manifestations, drastic changes in mood, new pains or changes in joint pains, often but not always in the neck, back, knee or elbow.
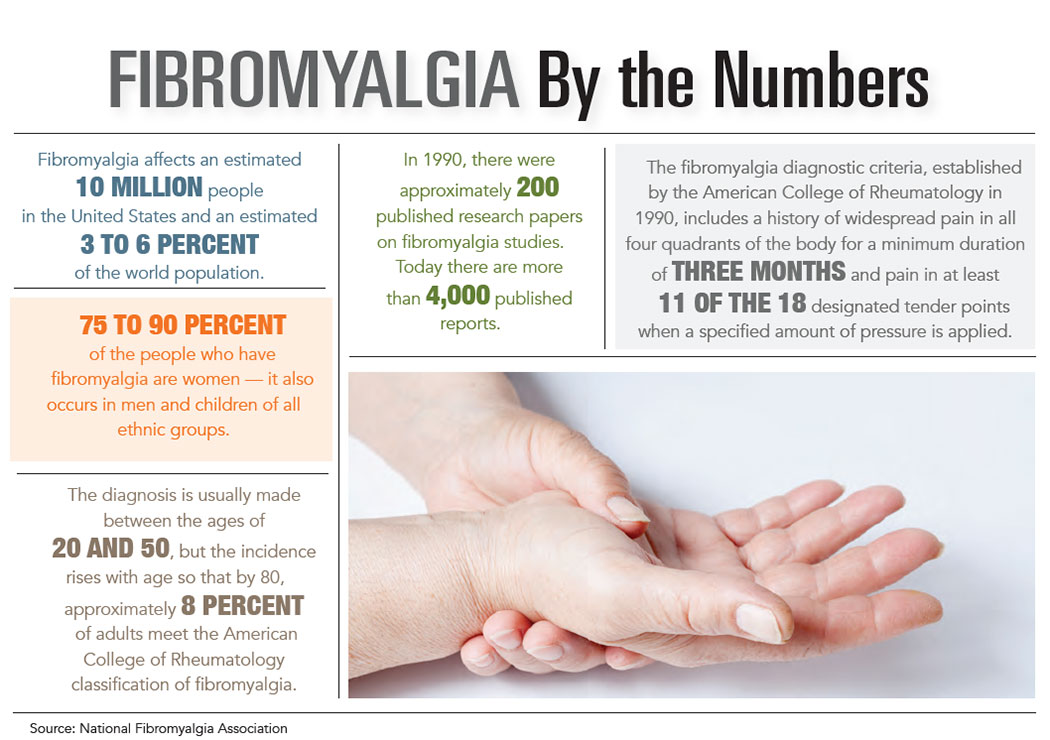
On some days, I feel like I’m in a pit of despair and that no one truly understands my pain – and I’m sure those of you suffering from fibromyalgia sometimes have the same attitude. However, after digging into the facts, I’ve realized that it is one of the most common – and perhaps one of the most misunderstood – chronic health conditions, with an estimated 10 million people affected by fibromyalgia in the United States. So while it’s an invisible, “noncurable” disease, it is manageable. More importantly, you and I are not alone.
By Helen Harris